Discovering LTB: A Protein Involved in Inflammation (G4050)
Discovering LTB: A Protein Involved in Inflammation
Tumor necrosis factor ligand (TNFL) 1C (also known as LTB) is a protein that is expressed in a variety of tissues, including the liver, spleen, and peripheral blood cells. It is a potent stimulator of the production of pro-inflammatory cytokines, which play a key role in the regulation of immune and inflammatory responses. In recent years, researchers have become increasingly interested in the potential clinical applications of LTB as a drug target or biomarker.
The discovery and characterization of LTB was made by a team of researchers led by Dr. David S. Wishart at the University of Alberta. In 2002, they identified a novel protein that was highly expressed in the liver and spleen, and named it LTB. They found that LTB was highly sensitive to inhibition by small molecules, which suggested that it might be a good candidate for a drug. The team then went on to conduct a series of experiments to confirm that their hypothesis was correct.
The first experiment they conducted was a high-throughput screening experiment, which involved the screening of a library of small molecules for their ability to inhibit LTB activity. They found that a number of small molecules, including inhibitors of the tyrosine kinase pathway, were able to inhibit LTB activity. This was unexpected, as inhibitors of this pathway were not expected to be effective in inhibiting LTB activity.
The next experiment that the team conducted was a biochemical assay of LTB activity. They found that inhibitors of LTB activity were able to decrease the amount of inflammatory cytokines that were produced by mouse peritoneal macrophages, which are a type of immune cell that are responsible for producing pro-inflammatory cytokines. This was consistent with the idea that LTB is involved in the regulation of inflammatory responses.
The team also conducted a series of functional studies to further validate the potential clinical applications of LTB as an inhibitor of pro-inflammatory cytokines. They found that inhibitors of LTB activity were able to protect against the development of experimental autoimmune disease (EAD) in mice, which is a type of disease in which the immune system attacks the body's own tissues. This suggests that LTB may be a potential therapeutic target for EAD.
In addition to its potential clinical applications, LTB has also generated a lot of interest as a drug target. Many researchers are actively working on developing inhibitors of LTB activity, with the goal of using these inhibitors to treat a variety of diseases. For example, some researchers are investigating the potential of inhibitors of LTB activity to treat autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis.
Another potential application of LTB is its potential as a biomarker. Because LTB is highly expressed in a variety of tissues, it may be a useful marker for tracking the development of certain diseases. For example, researchers are using LTB as a biomarker to diagnose and monitor the progression of multiple sclerosis, a progressive autoimmune disease.
In conclusion, LTB is a protein that is expressed in a variety of tissues and is involved in the regulation of inflammatory responses. In recent years, researchers have become increasingly interested in the potential clinical applications of LTB as an inhibitor of pro-inflammatory cytokines. The team has found that inhibitors of LTB activity are able to decrease the production of inflammatory cytokines and protect against the development of experimental autoimmune disease. In addition to its potential clinical applications, LTB has also generated a lot of interest as a drug target and as a biomarker. Further research is needed to fully understand the potential of LTB as a therapeutic
Protein Name: Lymphotoxin Beta
Functions: Cytokine that binds to LTBR/TNFRSF3. May play a specific role in immune response regulation. Provides the membrane anchor for the attachment of the heterotrimeric complex to the cell surface. Isoform 2 is probably non-functional
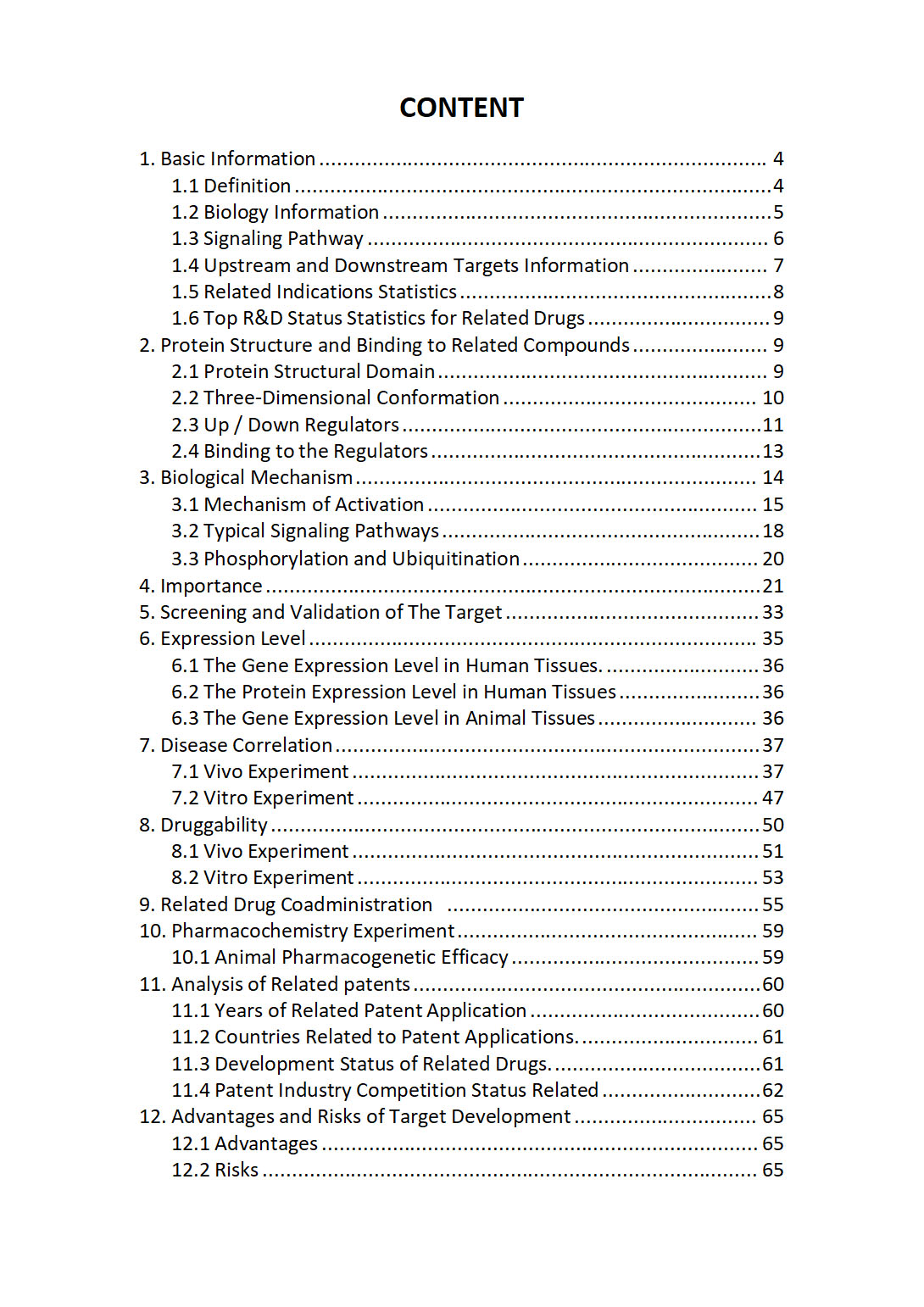
The "LTB Target / Biomarker Review Report" is a customizable review of hundreds up to thousends of related scientific research literature by AI technology, covering specific information about LTB comprehensively, including but not limited to:
• general information;
• protein structure and compound binding;
• protein biological mechanisms;
• its importance;
• the target screening and validation;
• expression level;
• disease relevance;
• drug resistance;
• related combination drugs;
• pharmacochemistry experiments;
• related patent analysis;
• advantages and risks of development, etc.
The report is helpful for project application, drug molecule design, research progress updates, publication of research papers, patent applications, etc. If you are interested to get a full version of this report, please feel free to contact us at BD@silexon.ai
More Common Targets
LTB4R | LTB4R2 | LTBP1 | LTBP2 | LTBP3 | LTBP4 | LTBR | LTC4S | LTF | LTK | LTN1 | LTO1 | LTV1 | LUADT1 | LUC7L | LUC7L2 | LUC7L3 | LUCAT1 | LUM | LUNAR1 | LURAP1 | LURAP1L | LURAP1L-AS1 | Luteinizing hormone | LUZP1 | LUZP2 | LUZP4 | LUZP6 | LVRN | LXN | LY6D | LY6E | LY6E-DT | LY6G5B | LY6G5C | LY6G6C | LY6G6D | LY6G6E | LY6G6F | LY6H | LY6K | LY75 | LY75-CD302 | LY86 | LY86-AS1 | LY9 | LY96 | LYAR | LYG1 | LYG2 | LYL1 | Lymphocyte antigen 6 complex | LYN | LYNX1 | LYPD1 | LYPD2 | LYPD3 | LYPD4 | LYPD5 | LYPD6 | LYPD6B | LYPD8 | LYPLA1 | LYPLA2 | LYPLA2P1 | LYPLA2P2 | LYPLAL1 | LYPLAL1-AS1 | LYRM1 | LYRM2 | LYRM4 | LYRM4-AS1 | LYRM7 | LYRM9 | LYSET | Lysine-Specific Demethylase 3 | Lysine-specific demethylase 5 | LYSMD1 | LYSMD2 | LYSMD3 | LYSMD4 | Lysophospholipid (edg) Receptors | LYST | Lysyl Oxidase Homolog | LYVE1 | LYZ | LYZL1 | LYZL2 | LYZL4 | LYZL6 | LZIC | LZTFL1 | LZTR1 | LZTS1 | LZTS1-AS1 | LZTS2 | LZTS3 | m-Calpain | M1AP | M6PR