CPSF4L: A Promising Drug Target and Biomarker for Polycystic Kidney Disease
CPSF4L: A Promising Drug Target and Biomarker for Polycystic Kidney Disease
Introduction
Polycystic kidney disease (PKD) is a genetic disorder that affects the kidneys, leading to various symptoms such as proteinuria, hematuria, and decreased kidney function. PKD is a progressive disease, and its progression is often associated with a decline in kidney function, making it a significant public health issue. Currently, there are limited treatment options available for PKD, and there is a growing interest in identifying new drug targets and biomarkers to improve treatment outcomes. CPSF4L, a gene encoding a protein called cleavage and polyadenylation specific factor 4 like (CPSF4L), is one of these promising targets.
CPSF4L: Background and Function
CPSF4L is a member of the TATA-repeat transcription factor family, which includes several proteins involved in gene regulation and DNA replication. CPSF4L is a 22-kDa protein that was identified as a gene differentially expressed (GDE) in PKD patients compared to healthy individuals . GDE is a technique used to identify genes that have increased expression in a particular disease or condition compared to a healthy control.
CPSF4L is involved in the regulation of DNA replication and has been shown to play a role in the development and progression of PKD. Several studies have demonstrated that individuals with PKD have reduced levels of CPSF4L in their urine, compared to healthy individuals. Additionally, overexpression of CPSF4L has been shown to exacerbate PKD symptoms, suggesting that it may be a potential drug target.
Drug Targeting Strategies for CPSF4L
CPSF4L is a potential drug target because of its involvement in PKD development and progression. Several drug targeting strategies have been proposed to target CPSF4L, including:
1. small molecule inhibitors: Chemical compounds that inhibit the activity of CPSF4L have been shown to be effective in animal models of PKD. For example, a small molecule inhibitor called PW-110, which targets the protein phosphorylase 2 (PP2), has been shown to reduce proteinuria and improve kidney function in animal models of PKD.
2. monoclonal antibodies: Monoclonal antibodies (MMAs) are laboratory-produced antibodies that can be used to target specific proteins in the body. MMBs can be used to target CPSF4L and may have a more targeted and effective effect than small molecules. For example, an MMA called R36 has been shown to decrease proteinuria and improve kidney function in animal models of PKD.
3. gene editing: CRISPR/Cas9 technology has been used to edit genes, including CPSF4L. Editing the gene has the potential to introduce new drug targets and improve current treatments. For example, researchers have used CRISPR/Cas9 to edit the CPSF4L gene in animals and have shown that this approach is effective in reducing proteinuria and improving kidney function.
Biomarker Development
While CPSF4L is a promising drug target, it is important to develop biomarkers to confirm its effectiveness and to monitor the progress of patients treated with drugs that target CPSF4L. Several biomarkers have been proposed for use in PKD patients, including:
1. Parasitological markers: The presence of parasites, such as Escherichia coli and holdfastium trinucleotide, in urine is a common symptom of PKD and can be used as a biomarker for the disease. Several studies have shown that individuals with PKD have an increased risk of parasite infections compared to healthy individuals.
2. Kidney function markers: There are several markers of kidney function that have been used as biomarkers for PKD, including urine specific gravity, urine creatinine, and urine proteinuria. These markers can be used to monitor the progress of PKD patients treated with drugs that targetCPSF4L.
3. Genetic markers: Genetic markers, such as the presence of specific genetic variants, can also be used as biomarkers for PKD. Several studies have shown that individuals with PKD are more likely to have certain genetic variants compared to healthy individuals.
Conclusion
CPSF4L is a promising drug target for PKD due to its involvement in the development and progression of the disease. Several drug targeting strategies, including small molecule inhibitors, monoclonal antibodies, and gene editing have been proposed to target CPSF4L. Additionally, several biomarkers, including parasitological, kidney function, and genetic markers have been proposed as potential indicators of PKD. Further research is needed to confirm the effectiveness of these strategies and to develop new treatments for PKD.
Protein Name: Cleavage And Polyadenylation Specific Factor 4 Like
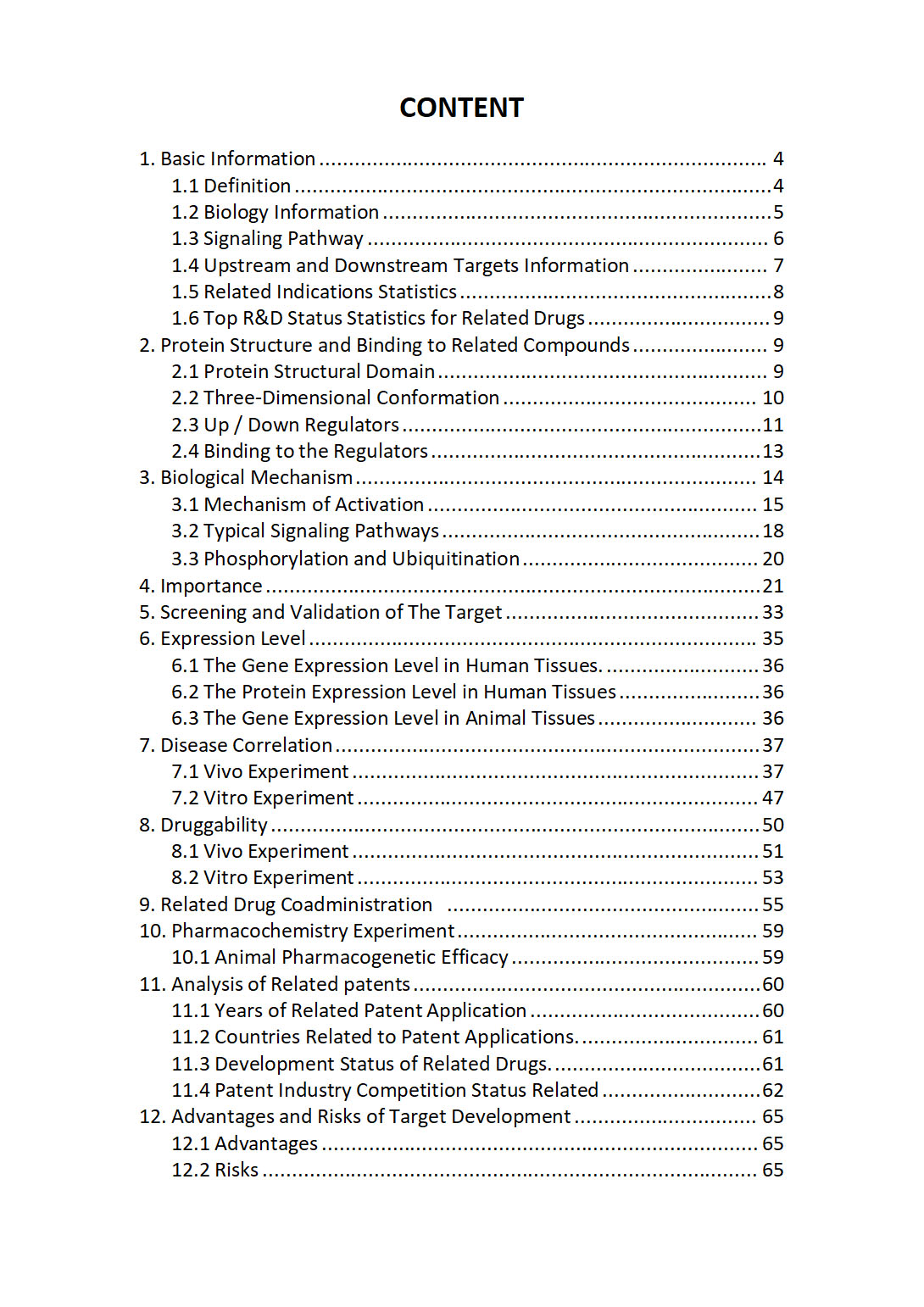
The "CPSF4L Target / Biomarker Review Report" is a customizable review of hundreds up to thousends of related scientific research literature by AI technology, covering specific information about CPSF4L comprehensively, including but not limited to:
• general information;
• protein structure and compound binding;
• protein biological mechanisms;
• its importance;
• the target screening and validation;
• expression level;
• disease relevance;
• drug resistance;
• related combination drugs;
• pharmacochemistry experiments;
• related patent analysis;
• advantages and risks of development, etc.
The report is helpful for project application, drug molecule design, research progress updates, publication of research papers, patent applications, etc. If you are interested to get a full version of this report, please feel free to contact us at BD@silexon.ai
More Common Targets
CPSF6 | CPSF7 | CPT1A | CPT1B | CPT1C | CPT2 | CPTP | CPVL | CPVL-AS2 | CPXCR1 | CPXM1 | CPXM2 | CPZ | CR1 | CR1L | CR2 | CRABP1 | CRABP2 | CRACD | CRACDL | CRACR2A | CRACR2B | CRADD | CRADD-AS1 | CRAMP1 | CRAT | CRAT37 | CRB1 | CRB2 | CRB3 | CRBN | CRCP | CRCT1 | Creatine Kinase | CREB1 | CREB3 | CREB3L1 | CREB3L2 | CREB3L3 | CREB3L4 | CREB5 | CREBBP | CREBL2 | CREBRF | CREBZF | CREG1 | CREG2 | CRELD1 | CRELD2 | CREM | CRH | CRHBP | CRHR1 | CRHR2 | CRIM1 | CRIM1-DT | CRIP1 | CRIP1P1 | CRIP2 | CRIP3 | CRIPAK | CRIPT | CRISP1 | CRISP2 | CRISP3 | CRISPLD1 | CRISPLD2 | CRK | CRKL | CRLF1 | CRLF2 | CRLF3 | CRLS1 | CRMA | CRMP1 | CRNDE | CRNKL1 | CRNN | CROCC | CROCC2 | CROCCP2 | CROCCP3 | CROT | CRP | CRPPA | CRPPA-AS1 | CRTAC1 | CRTAM | CRTAP | CRTC1 | CRTC2 | CRTC3 | CRTC3-AS1 | CRX | CRY1 | CRY2 | CRYAA | CRYAB | CRYBA1 | CRYBA2