BTLA as A Drug Target for Leukemia and Solid Tumors (G151888)
BTLA as A Drug Target for Leukemia and Solid Tumors
BTLA (B cell type-1 like acute leukemia) is a type of acute leukemia that affects the bone marrow and blood cells. It is characterized by the production of a specific type of leukemia cell called blasts, which are abnormal white blood cells that are not part of the normal immune system.
BTLA is a protein that is expressed in the blood cells, including blasts. It is a key regulator of the development and proliferation of these leukemia cells, and it is thought to play a role in the development of many different types of leukemia.
Recent studies have suggested that BTLA may be a drug target for the treatment of BTLA-positive solid tumors. In these studies, researchers have found that BTLA is often expressed in the tumors, and that inhibiting its activity may be a way to treat these tumors.
Another potential use for BTLA as a drug target is its role in the development of BTLA-positive relapse after cancer treatment. In these cases, BTLA may help to protect the cancer cells from being defeated by the immune system, leading to the development of relapse.
BTLA has also been shown to be involved in the development of BTLA-positive acute myeloid leukemias (AMLs), a type of cancer that affects the bone marrow and blood cells. In these cases, BTLA may contribute to the development of the leukemia by regulating the production of normal blood cells.
In addition to its potential as a drug target, BTLA has also been shown to be involved in the development of BTLA-positive chronic myeloid leukemias (CMLs), another type of cancer that affects the bone marrow and blood cells. In these cases, BTLA may contribute to the development of the leukemia by regulating the production of normal blood cells.
Despite the potential benefits of BTLA as a drug target, there are also concerns about its safety and potential side effects. For example, BTLA has been shown to be involved in the development of anemia in cancer patients, and it is possible that inhibiting its activity may cause this side effect.
In addition, there are also concerns about the long-term effects of BTLA inhibitors on the immune system. For example, BTLA has been shown to play a role in regulating the immune response, and it is possible that inhibiting its activity may affect the body's ability to fight off infections.
Overall, while BTLA has the potential to be a drug target for the treatment of BTLA-positive solid tumors and BTLA-positive relapse after cancer treatment, further research is needed to fully understand its role and potential safety.
Protein Name: B And T Lymphocyte Associated
Functions: Inhibitory receptor on lymphocytes that negatively regulates antigen receptor signaling via PTPN6/SHP-1 and PTPN11/SHP-2 (PubMed:12796776, PubMed:14652006, PubMed:15568026, PubMed:18193050). May interact in cis (on the same cell) or in trans (on other cells) with TNFRSF14 (PubMed:19915044). In cis interactions, appears to play an immune regulatory role inhibiting in trans interactions in naive T cells to maintain a resting state. In trans interactions, can predominate during adaptive immune response to provide survival signals to effector T cells (PubMed:19915044)
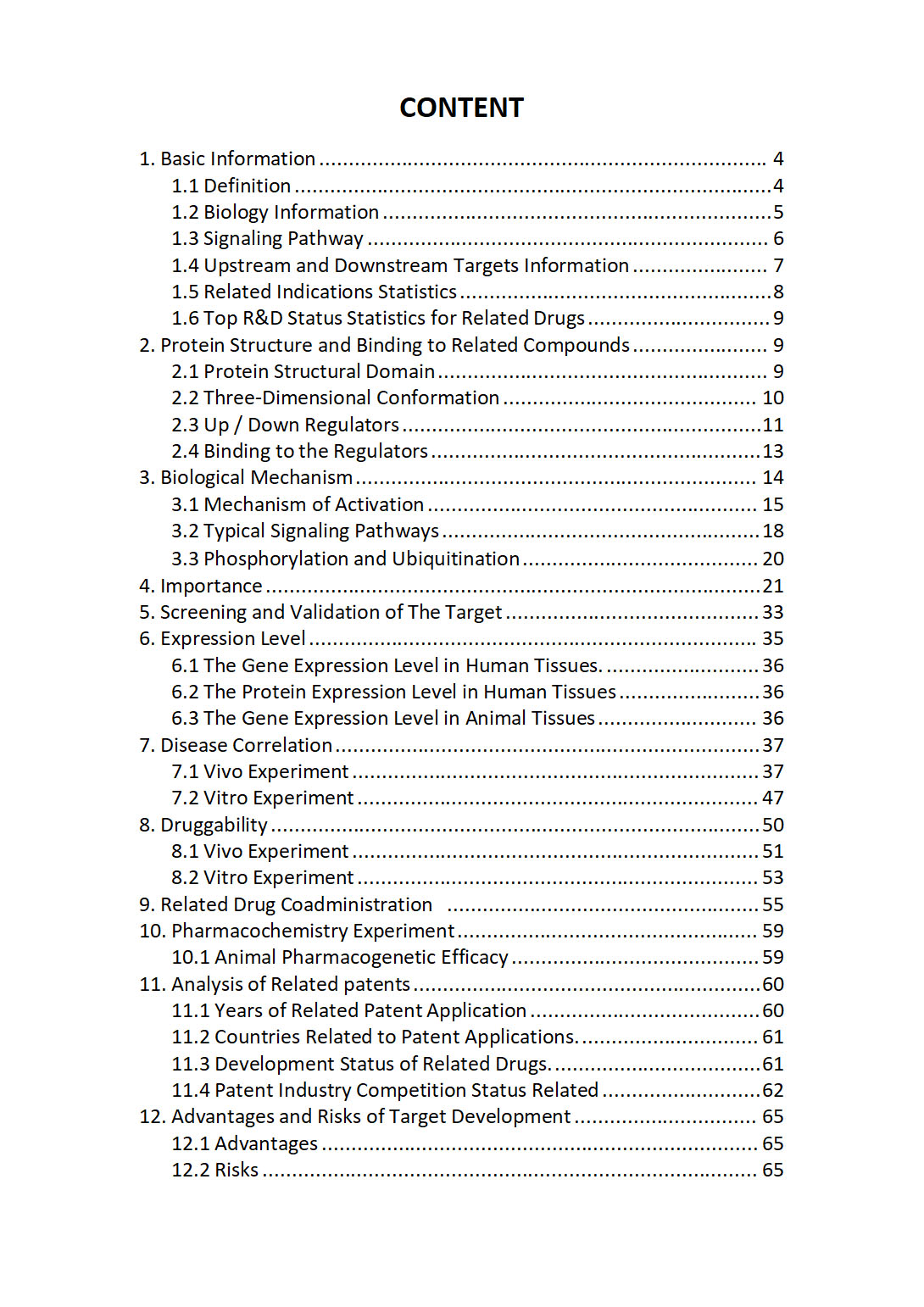
The "BTLA Target / Biomarker Review Report" is a customizable review of hundreds up to thousends of related scientific research literature by AI technology, covering specific information about BTLA comprehensively, including but not limited to:
• general information;
• protein structure and compound binding;
• protein biological mechanisms;
• its importance;
• the target screening and validation;
• expression level;
• disease relevance;
• drug resistance;
• related combination drugs;
• pharmacochemistry experiments;
• related patent analysis;
• advantages and risks of development, etc.
The report is helpful for project application, drug molecule design, research progress updates, publication of research papers, patent applications, etc. If you are interested to get a full version of this report, please feel free to contact us at BD@silexon.ai
More Common Targets
BTN1A1 | BTN2A1 | BTN2A2 | BTN2A3P | BTN3A1 | BTN3A2 | BTN3A3 | BTNL10P | BTNL2 | BTNL3 | BTNL8 | BTNL9 | BTRC | BUB1 | BUB1B | BUB1B-PAK6 | BUB3 | BUD13 | BUD23 | BUD31 | Butyrophilin | Butyrophilin subfamily 3 member A (BTN3A) | BVES | BVES-AS1 | BYSL | BZW1 | BZW1-AS1 | BZW1P2 | BZW2 | C-C chemokine receptor | C10orf105 | C10orf113 | C10orf120 | C10orf126 | C10orf143 | C10orf53 | C10orf55 | C10orf62 | C10orf67 | C10orf71 | C10orf71-AS1 | C10orf82 | C10orf88 | C10orf88B | C10orf90 | C10orf95 | C10orf95-AS1 | C11orf16 | C11orf21 | C11orf24 | C11orf40 | C11orf42 | C11orf52 | C11orf54 | C11orf58 | C11orf65 | C11orf68 | C11orf71 | C11orf80 | C11orf86 | C11orf87 | C11orf91 | C11orf96 | C11orf97 | C11orf98 | C12orf29 | C12orf4 | C12orf40 | C12orf42 | C12orf43 | C12orf50 | C12orf54 | C12orf56 | C12orf57 | C12orf60 | C12orf74 | C12orf75 | C12orf76 | C13orf42 | C13orf46 | C14orf119 | C14orf132 | C14orf178 | C14orf180 | C14orf28 | C14orf39 | C14orf93 | C15orf32 | C15orf39 | C15orf40 | C15orf48 | C15orf61 | C15orf62 | C16orf46 | C16orf54 | C16orf74 | C16orf78 | C16orf82 | C16orf86 | C16orf87