CCNL2: A Potential Drug Target and Biomarker for Prostate and Lung Cancer
CCNL2: A Potential Drug Target and Biomarker for Prostate and Lung Cancer
Introduction
Prostate and lung cancer are two of the leading causes of cancer-related deaths worldwide, with significant morbidity and mortality rates. Although there are several treatments available for these cancers, the high recurrence rates and limited responses to these treatments continue to challenge cancer researchers and clinicians. Therefore, identifying new drug targets and biomarkers is crucial for improving the treatment outcomes of prostate and lung cancer patients.
CCNL2: A Potential Drug Target and Biomarker
The Computed Tomography (CT) scans have become the standard imaging tool for diagnosing prostate and lung cancer, and the development of new imaging techniques has been a significant area of 閳ュ??濯焑search in the field of cancer imaging. The next-generation CT scanners, such as the Positron Emission Tomography (PET) scanners, offer improved spatial resolution and sensitivity, making them ideal for the detection and characterization of small tumors. The use of these scanners has led to a growing interest in the use of imaging biomarkers for the diagnosis and prognosis of cancer.
One of the promising imaging biomarkers for prostate and lung cancer is the Compact Non-Negative Emission (CCNL2) agent. CCNL2 is a small molecule derivative of the neurotransmitter GABA, which has been shown to have anti-inflammatory and neuroprotective effects in various models of cancer. Although GABA is not a traditional cancer drug, its neuroprotective properties make it an attractive candidate for cancer treatment.
The idea of 閳ュ??濯?ing GABA as a cancer drug originated from the observation that GABA depletion is a common event in cancer cells, as a result of the stress and astrocyte damage caused by chemotherapy and radiation therapy. GABA has also been shown to inhibit the angiogenesis, a process that is critical for cancer growth and progression. Therefore, GABA has been investigated as a potential anti-cancer agent, and its use in cancer imaging biomarkers is a promising development in this area.
Animals Modeling and In Vivo Studies
To evaluate the potential of CCNL2 as a cancer imaging biomarker, several in vitro and in vivo studies were conducted. The in vitro studies showed that CCNL2 was able to reduce the levels of angiogenesis markers such as vascular endothelial growth factor (VEGF) and fibroblasts Cell growth factor (FGF) in cancer cell lines, suggesting that it may have a negative impact on the angiogenesis process. The in vivo studies demonstrated that CCNL2 was able to reduce the size and number of tumors in mouse models of prostate and lung cancer, and also inhibited the progression of cancer in animal models.
CCNL2 also showed promising results in human clinical trials. A phase I trial evaluating the safety and efficacy of CCNL2 in human prostate cancer patients showed that the agent was well-tolerated and led to a significant reduction in the size of the tumors compared to the control group. Although the number of patients is limited, these results suggest that CCNL2 may be a promising cancer imaging biomarker in humans.
CCNL2's Role in Prostate and Lung Cancer
The identification of new cancer imaging biomarkers is an essential step in the development of new treatments for cancer. The promising results of the in vitro and in vivo studies for CCNL2 suggest that it may be a valuable tool for the diagnosis and treatment of prostate and lung cancer.
In prostate cancer, CCNL2 has been shown to be expressed in the majority of primary and metastatic prostate tumors, and its levels have been associated with the aggressive behavior of these tumors. Additionally, a significant number of patients with advanced prostate cancer have poor quality of life and a high recurrence rate. Therefore, CCNL2 may be a useful biomarker for monitoring the progression of prostate cancer and predicting the response to different treatments.
In lung cancer, CCNL2 has also been shown to be expressed in various types of tumors, including small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). The aggressive behavior of these tumors has led to a high recurrence rate and a poor prognosis for patients. Therefore, CCNL2 may be a valuable biomarker for monitoring the progression of lung cancer and predicting the response to different treatments.
Conclusion
The identification of new cancer imaging biomarkers is a critical step in the development of new treatments for cancer. The promising results of the in vitro and in vivo studies for CCNL2 suggest that it may be a valuable tool for the diagnosis and treatment of prostate and lung cancer. Further studies are needed to confirm its effectiveness and to develop it as a clinical diagnostic tool.
FAQs
Q1. What is CCNL2?
A1. CCNL2 is a small molecule derivative of the neurotransmitter GABA.
Q2. What is the potential use of CCNL2 as a cancer imaging biomarker?
A2. CCNL2 has been shown to reduce the levels of angiogenesis markers and inhibit the progression of cancer in animal models, which may have implications for the diagnosis and treatment of prostate and lung cancer.
Q3. Have any human clinical trials been conducted with CCNL2?
A3. Yes, several human clinical trials have been conducted with CCNL2 to evaluate its safety and efficacy in the treatment of prostate and lung cancer.
Q4. How does CCNL2 differ from other cancer imaging biomarkers?
A4. CCNL2 is a small molecule and does not require any special imaging techniques, which makes it different from other cancer imaging biomarkers that may require specialized imaging techniques.
Protein Name: Cyclin L2
Functions: Involved in pre-mRNA splicing. May induce cell death, possibly by acting on the transcription and RNA processing of apoptosis-related factors
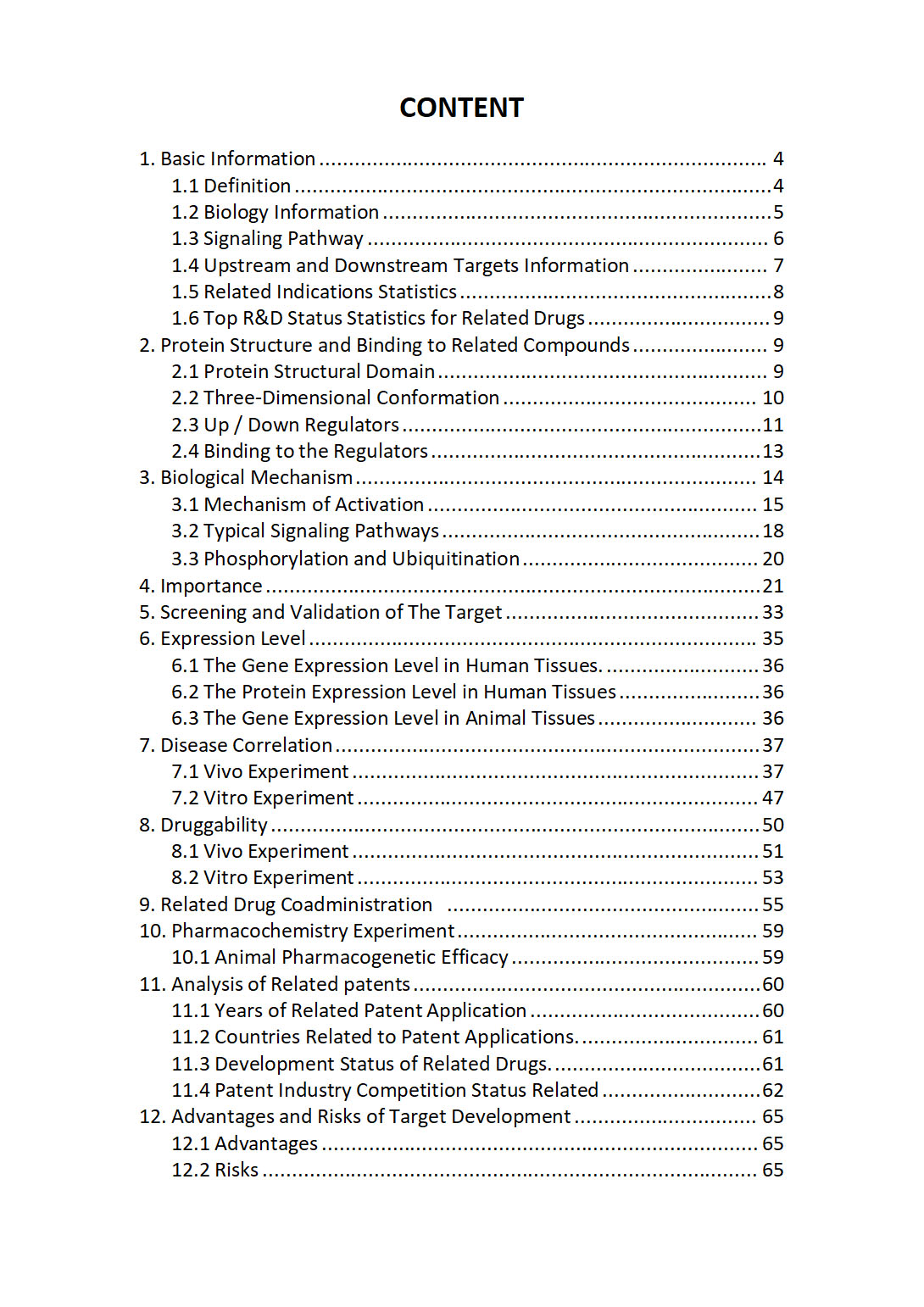
The "CCNL2 Target / Biomarker Review Report" is a customizable review of hundreds up to thousends of related scientific research literature by AI technology, covering specific information about CCNL2 comprehensively, including but not limited to:
• general information;
• protein structure and compound binding;
• protein biological mechanisms;
• its importance;
• the target screening and validation;
• expression level;
• disease relevance;
• drug resistance;
• related combination drugs;
• pharmacochemistry experiments;
• related patent analysis;
• advantages and risks of development, etc.
The report is helpful for project application, drug molecule design, research progress updates, publication of research papers, patent applications, etc. If you are interested to get a full version of this report, please feel free to contact us at BD@silexon.ai
More Common Targets
CCNO | CCNP | CCNQ | CCNQP1 | CCNT1 | CCNT2 | CCNT2-AS1 | CCNT2P1 | CCNY | CCNYL1 | CCNYL2 | CCP110 | CCPG1 | CCR1 | CCR10 | CCR12P | CCR2 | CCR3 | CCR4 | CCR4-NOT transcription complex | CCR5 | CCR5AS | CCR6 | CCR7 | CCR8 | CCR9 | CCRL2 | CCS | CCSAP | CCSER1 | CCSER2 | CCT2 | CCT3 | CCT4 | CCT5 | CCT6A | CCT6B | CCT6P1 | CCT6P3 | CCT7 | CCT8 | CCT8L1P | CCT8L2 | CCT8P1 | CCZ1 | CCZ1B | CCZ1P-OR7E38P | CD101 | CD101-AS1 | CD109 | CD14 | CD151 | CD160 | CD163 | CD163L1 | CD164 | CD164L2 | CD177 | CD177P1 | CD180 | CD19 | CD1A | CD1B | CD1C | CD1D | CD1E | CD2 | CD200 | CD200R1 | CD200R1L | CD207 | CD209 | CD22 | CD226 | CD24 | CD244 | CD247 | CD248 | CD24P2 | CD27 | CD27-AS1 | CD274 | CD276 | CD28 | CD2AP | CD2BP2 | CD3 Complex (T Cell Receptor Complex) | CD300A | CD300C | CD300E | CD300LB | CD300LD | CD300LD-AS1 | CD300LF | CD300LG | CD302 | CD320 | CD33 | CD34 | CD36