TRPV4: A Potential Drug Target for Pain Management (G9971)
TRPV4: A Potential Drug Target for Pain Management
The Nuclear Receptor Subfamily 1 (NR1H4) is a gene that encodes a protein known as TRPV4, which is a member of the TRPV family of nuclear receptors. These proteins are involved in the signaling pathway that regulates pain, inflammation, and body temperature. TRPV4 is a G protein-coupled receptor (GPCR), which means that it interacts with intracellular signaling molecules called GPCRs.
The TRPV4 gene has four splice variants, which are responsible for generating different TRPV4 proteins with different amino acid sequences. One of these variants, known as TRPV4-308, has been shown to interact with the neurotransmitter called nitric oxide (NO) and to play a role in the regulation of blood flow to the brain. This variant is also known as NR1H4, which is the gene code for the protein it encodes.
Drug Targets and Biomarkers
TRPV4 has been identified as a potential drug target for the treatment of various neurological and psychiatric disorders, including chronic pain, neurodegenerative diseases, and autoimmune disorders. The ability of TRPV4 to modulate pain perception and blood flow to the brain makes it an attractive target for the development of pain medications.
One of the main advantages of TRPV4 as a drug target is its high degree of genetic variability. Unlike many other GPCRs, TRPV4 has a large number of different splice variants, which means that researchers can use a variety of approaches to target different variants of the gene. This makes it easier to identify potential drug candidates and to test their effectiveness.
Another advantage of TRPV4 is its location in the body. TRPV4 is expressed in many different tissues and organs, including the brain, heart, kidneys, and intestine. This makes it an attractive target for drugs that can affect multiple organs and tissues.
TRPV4 has also been shown to be involved in the regulation of pain perception and emotion. Studies have shown that TRPV4 interacts with the neurotransmitter NO and that it is involved in the regulation of pain sensitivity. This suggests that TRPV4 may be a useful target for the treatment of chronic pain conditions.
In addition to its potential as a drug target, TRPV4 has also been identified as a potential biomarker for the assessment of pain and inflammation. The ability of TRPV4 to modulate pain perception and blood flow to the brain makes it an attractive target for the development of pain and inflammation biomarkers.
Methods
To study the potential drug targets of TRPV4, researchers have used a variety of techniques, including in vitro and in vivo assays, animal models, and human clinical trials. One of the main assays used to study TRPV4 is the patch-electrode technique, which allows researchers to measure the electrical activity of individual neurons in the brain.
In vitro assays have been used to show that TRPV4 is involved in the regulation of pain perception and emotion. Studies have shown that TRPV4 interacts with the neurotransmitter NO and that it is involved in the regulation of pain sensitivity. In addition, studies have shown that TRPV4 is involved in the regulation of blood flow to the brain, which may be related to the regulation of pain perception.
In vivo assays have also been used to study TRPV4. For example, researchers have used techniques such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) to show that TRPV4 is involved in the regulation of pain perception and emotion in live animals. These studies have shown that TRPV4 interacts with the neurotransmitter NO and that it is involved in the regulation of pain sensitivity.
Animal models have also been used to study TRPV4. Researchers have shown that TRPV4 is involved in the regulation of pain perception and emotion in animals, and that the effects of pain medications can be influenced by the level of TRPV4 expression in the animal models.
Human clinical trials have also been used to study TRPV4. These studies have shown that TRPV4 is involved in the regulation of pain perception and emotion in humans, and that the effects of pain medications can be influenced by the level of TRPV4 expression in the human subjects.
Conclusion
In conclusion, TRPV4 is a gene that encodes a protein involved in the regulation of pain perception and emotion. Its high degree of genetic variability and its location in multiple tissues make it an attractive target for the development of pain medications. In addition, TRPV4 has also been shown to be involved in the regulation of blood flow to the brain, which may be related to the regulation of pain perception. Further research is needed to fully understand the role of TRPV4 as a drug target and biomarker.
Protein Name: Nuclear Receptor Subfamily 1 Group H Member 4
Functions: Ligand-activated transcription factor. Receptor for bile acids (BAs) such as chenodeoxycholic acid (CDCA), lithocholic acid, deoxycholic acid (DCA) and allocholic acid (ACA). Plays a essential role in BA homeostasis through the regulation of genes involved in BA synthesis, conjugation and enterohepatic circulation. Also regulates lipid and glucose homeostasis and is involved innate immune response (PubMed:10334992, PubMed:10334993, PubMed:21383957, PubMed:22820415). The FXR-RXR heterodimer binds predominantly to farnesoid X receptor response elements (FXREs) containing two inverted repeats of the consensus sequence 5'-AGGTCA-3' in which the monomers are spaced by 1 nucleotide (IR-1) but also to tandem repeat DR1 sites with lower affinity, and can be activated by either FXR or RXR-specific ligands. It is proposed that monomeric nuclear receptors such as NR5A2/LRH-1 bound to coregulatory nuclear responsive element (NRE) halfsites located in close proximity to FXREs modulate transcriptional activity (By similarity). In the liver activates transcription of the corepressor NR0B2 thereby indirectly inhibiting CYP7A1 and CYP8B1 (involved in BA synthesis) implicating at least in part histone demethylase KDM1A resulting in epigenomic repression, and SLC10A1/NTCP (involved in hepatic uptake of conjugated BAs). Activates transcription of the repressor MAFG (involved in regulation of BA synthesis) (By similarity). Activates transcription of SLC27A5/BACS and BAAT (involved in BA conjugation), ABCB11/BSEP (involved in bile salt export) by directly recruiting histone methyltransferase CARM1, and ABCC2/MRP2 (involved in secretion of conjugated BAs) and ABCB4 (involved in secretion of phosphatidylcholine in the small intestine) (PubMed:12754200, PubMed:15471871, PubMed:17895379). Activates transcription of SLC27A5/BACS and BAAT (involved in BA conjugation), ABCB11/BSEP (involved in bile salt export) by directly recruiting histone methyltransferase CARM1, and ABCC2/MRP2 (involved in secretion of conjugated BAs) and ABCB4 (involved in secretion of phosphatidylcholine in the small intestine) (PubMed:10514450, PubMed:15239098, PubMed:16269519). In the intestine activates FGF19 expression and secretion leading to hepatic CYP7A1 repression (PubMed:12815072, PubMed:19085950). The function also involves the coordinated induction of hepatic KLB/beta-klotho expression (By similarity). Regulates transcription of liver UGT2B4 and SULT2A1 involved in BA detoxification; binding to the UGT2B4 promoter seems to imply a monomeric transactivation independent of RXRA (PubMed:12806625, PubMed:16946559). Modulates lipid homeostasis by activating liver NR0B2/SHP-mediated repression of SREBF1 (involved in de novo lipogenesis), expression of PLTP (involved in HDL formation), SCARB1 (involved in HDL hepatic uptake), APOE, APOC1, APOC4, PPARA (involved in beta-oxidation of fatty acids), VLDLR and SDC1 (involved in the hepatic uptake of LDL and IDL remnants), and inhibiting expression of MTTP (involved in VLDL assembly (PubMed:12660231, PubMed:12554753, PubMed:15337761). Increases expression of APOC2 (promoting lipoprotein lipase activity implicated in triglyceride clearance) (PubMed:11579204). Transrepresses APOA1 involving a monomeric competition with NR2A1 for binding to a DR1 element (PubMed:11927623, PubMed:21804189). Also reduces triglyceride clearance by inhibiting expression of ANGPTL3 and APOC3 (both involved in inhibition of lipoprotein lipase) (PubMed:12891557). Involved in glucose homeostasis by modulating hepatic gluconeogenesis through activation of NR0B2/SHP-mediated repression of respective genes. Modulates glycogen synthesis (inducing phosphorylation of glycogen synthase kinase-3) (By similarity). Modulates glucose-stimulated insulin secretion and is involved in insulin resistance (PubMed:20447400). Involved in intestinal innate immunity. Plays a role in protecting the distal small intestine against bacterial overgrowth and preservation of the epithelial barrier (By similarity). Down-regulates inflammatory cytokine expression in several types of immune cells including macrophages and mononuclear cells (PubMed:21242261). Mediates trans-repression of TLR4-induced cytokine expression; the function seems to require its sumoylation and prevents N-CoR nuclear receptor corepressor clearance from target genes such as IL1B and NOS2 (PubMed:19864602). Involved in the TLR9-mediated protective mechanism in intestinal inflammation. Plays an anti-inflammatory role in liver inflammation; proposed to inhibit pro-inflammatory (but not antiapoptotic) NF-kappa-B signaling) (By similarity)
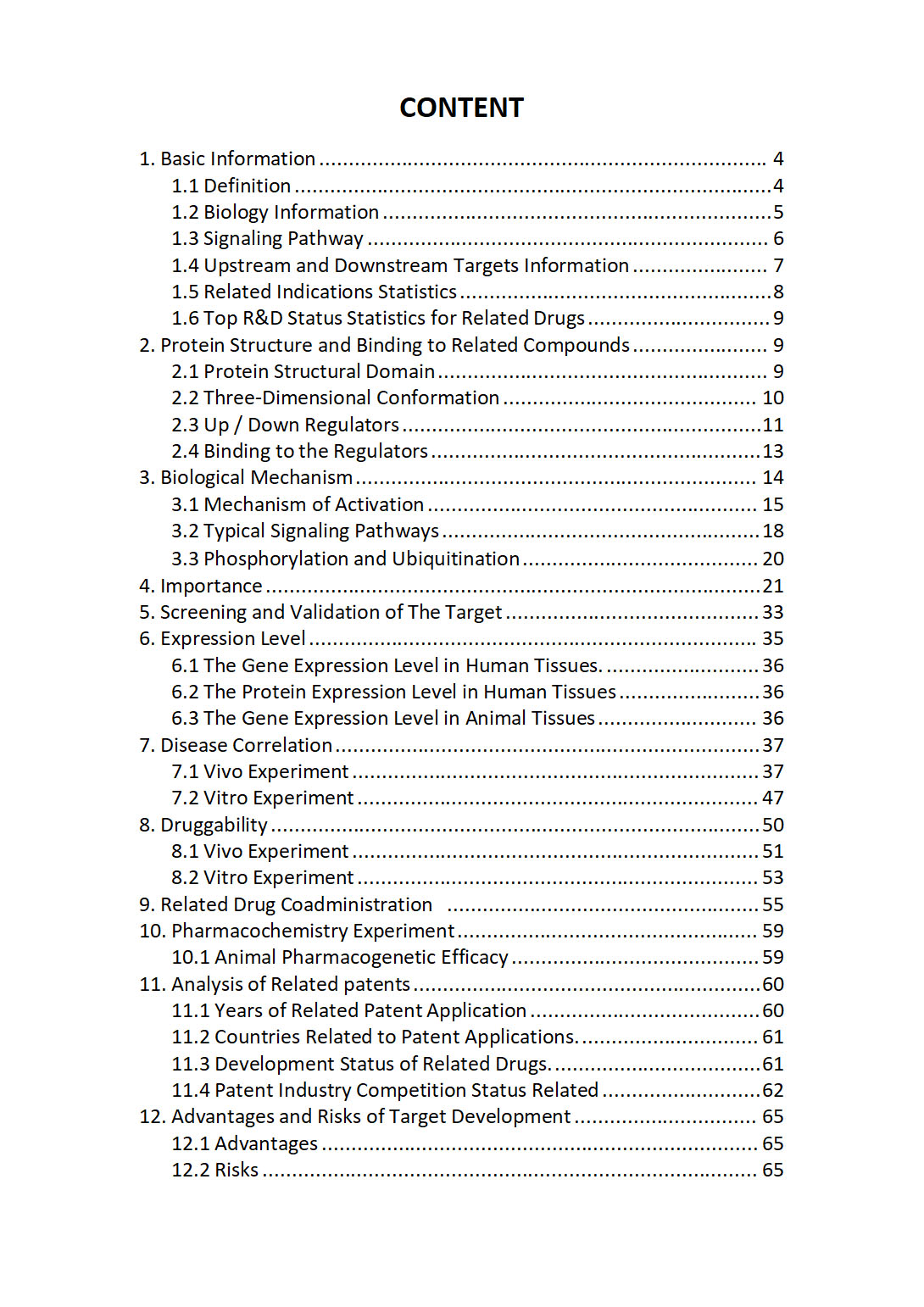
The "NR1H4 Target / Biomarker Review Report" is a customizable review of hundreds up to thousends of related scientific research literature by AI technology, covering specific information about NR1H4 comprehensively, including but not limited to:
• general information;
• protein structure and compound binding;
• protein biological mechanisms;
• its importance;
• the target screening and validation;
• expression level;
• disease relevance;
• drug resistance;
• related combination drugs;
• pharmacochemistry experiments;
• related patent analysis;
• advantages and risks of development, etc.
The report is helpful for project application, drug molecule design, research progress updates, publication of research papers, patent applications, etc. If you are interested to get a full version of this report, please feel free to contact us at BD@silexon.ai
More Common Targets
NR1I2 | NR1I3 | NR2C1 | NR2C2 | NR2C2AP | NR2E1 | NR2E3 | NR2F1 | NR2F1-AS1 | NR2F2 | NR2F2-AS1 | NR2F6 | NR3C1 | NR3C2 | NR4A1 | NR4A2 | NR4A3 | NR5A1 | NR5A2 | NR6A1 | NRAD1 | NRADDP | NRAP | NRARP | NRAS | NRAV | NRBF2 | NRBF2P4 | NRBP1 | NRBP2 | NRCAM | NRDC | NRDE2 | NREP | NRF1 | NRG1 | NRG2 | NRG3 | NRG4 | NRGN | NRIP1 | NRIP2 | NRIP3 | NRIP3-DT | NRIR | NRK | NRL | NRM | NRN1 | NRN1L | NRON | NRP1 | NRP2 | NRROS | NRSN1 | NRSN2 | NRSN2-AS1 | NRTN | NRXN1 | NRXN2 | NRXN2-AS1 | NRXN3 | NSA2 | NSA2P2 | NSD1 | NSD2 | NSD3 | NSDHL | NSF | NSFL1C | NSFP1 | NSG1 | NSG2 | NSL complex | NSL1 | NSMAF | NSMCE1 | NSMCE1-DT | NSMCE2 | NSMCE3 | NSMCE4A | NSMF | NSRP1 | NSUN2 | NSUN3 | NSUN4 | NSUN5 | NSUN5P1 | NSUN5P2 | NSUN6 | NSUN7 | NT5C | NT5C1A | NT5C1B | NT5C1B-RDH14 | NT5C2 | NT5C3A | NT5C3AP1 | NT5C3B | NT5CP2