TRBV17: A Potential Drug Target and Biomarker for T Cell Receptor灏? Variant 17
TRBV17: A Potential Drug Target and Biomarker for T Cell Receptor灏? Variant 17
Abstract:
T cell receptor (TCR)灏? variable 17 (TRBV17) is a highly polymorphic non-coding RNA molecule that plays a crucial role in T cell development, activation, and homeostasis. TRBV17 has been implicated in various autoimmune diseases, including rheumatoid arthritis (RA ), lupus, and multiple sclerosis. In this article, we review the current understanding of TRBV17, its potential drug targets, and its role as a biomarker in these diseases.
Introduction:
T cells are a vital immune cell that play a critical role in defending against infections and cancer. T cell receptor (TCR)灏? variable 17 (TRBV17) is a key molecule that regulates T cell development, activation, and homeostasis. TRBV17 is a non -coding RNA molecule that has been shown to participate in various TCR-related processes, including DNA replication, gene expression, and cell survival.
Disease association:
TRBV17 has been implicated in various autoimmune diseases, including RA, lupus, and multiple sclerosis. In rheumatoid arthritis (RA), TRBV17 has been shown to be overexpressed in the synovial tissue, and it has been associated with the development of joint damage and higher disease activity. In lupus, TRBV17 has been shown to be expressed in the T cells and to be involved in the development of immune-mediated diseases. In multiple sclerosis, TRBV17 has been shown to be overexpressed in the central nervous system and to be involved in the pathogenesis of this disease.
Potential drug targets:
TRBV17 is a potential drug target for treating autoimmune diseases. Several studies have shown that inhibiting TRBV17 can reduce the expression of anti-self CD4+ T cells and improve the body's immune response to foreign antigens. In addition, TRBV17 has been shown to be involved in the regulation of immune cell function, including the production of T regulatory cells. Therefore, TRBV17 may be a promising target for the development of new anti-autoimmune drugs.
Biomarkers:
TRBV17 has also been shown to be a potential biomarker for monitoring the efficacy of anti-autoimmune drugs. In several studies, researchers have shown that the levels of TRBV17 have been altered in patients with autoimmune diseases, and that these levels can be used as a marker for the efficacy of new treatments. Therefore, TRBV17 may be a valuable biomarker for the evaluation of the effectiveness of new anti-autoimmune drugs.
Conclusion:
In conclusion, TRBV17 is a non-coding RNA molecule that plays a crucial role in T cell development, activation, and homeostasis. Its involvement in various autoimmune diseases, including RA, lupus, and multiple sclerosis, makes it a promising target for the development of new drugs. In addition, TRBV17 has also been shown to be a potential biomarker for monitoring the efficacy of anti-autoimmune drugs. Further research is needed to fully understand the role of TRBV17 in these diseases and to develop new treatments based on this knowledge .
Protein Name: T Cell Receptor Beta Variable 17 (non-functional)
Functions: Probable non-functional open reading frame (ORF) of V region of the variable domain of T cell receptor (TR) beta chain (PubMed:24600447). Non-functional ORF generally cannot participate in the synthesis of a productive T cell receptor (TR) chain due to altered V-(D)-J or switch recombination and/or splicing site (at mRNA level) and/or conserved amino acid change (protein level) (PubMed:9619395). Alpha-beta T cell receptors are antigen specific receptors which are essential to the immune response and are present on the cell surface of T lymphocytes. Recognize peptide-major histocompatibility (MH) (pMH) complexes that are displayed by antigen presenting cells (APC), a prerequisite for efficient T cell adaptive immunity against pathogens (PubMed:25493333). Binding of alpha-beta TR to pMH complex initiates TR-CD3 clustering on the cell surface and intracellular activation of LCK that phosphorylates the ITAM motifs of CD3G, CD3D, CD3E and CD247 enabling the recruitment of ZAP70. In turn ZAP70 phosphorylates LAT, which recruits numerous signaling molecules to form the LAT signalosome. The LAT signalosome propagates signal branching to three major signaling pathways, the calcium, the mitogen-activated protein kinase (MAPK) kinase and the nuclear factor NF-kappa-B (NF-kB) pathways, leading to the mobilization of transcription factors that are critical for gene expression and essential for T cell growth and differentiation (PubMed:23524462). The T cell repertoire is generated in the thymus, by V-(D)-J rearrangement. This repertoire is then shaped by intrathymic selection events to generate a peripheral T cell pool of self-MH restricted, non-autoaggressive T cells. Post-thymic interaction of alpha-beta TR with the pMH complexes shapes TR structural and functional avidity (PubMed:15040585)
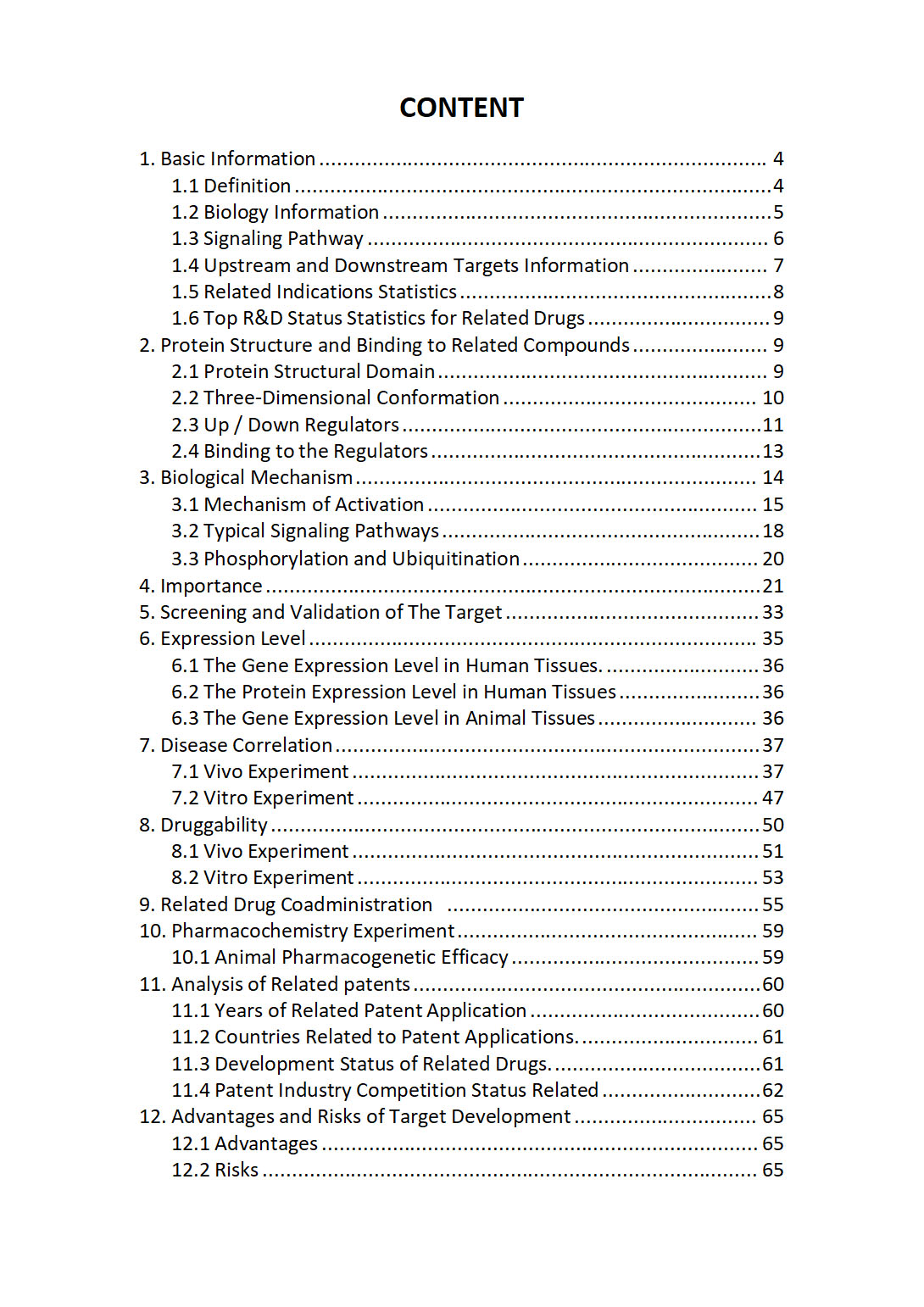
The "TRBV17 Target / Biomarker Review Report" is a customizable review of hundreds up to thousends of related scientific research literature by AI technology, covering specific information about TRBV17 comprehensively, including but not limited to:
• general information;
• protein structure and compound binding;
• protein biological mechanisms;
• its importance;
• the target screening and validation;
• expression level;
• disease relevance;
• drug resistance;
• related combination drugs;
• pharmacochemistry experiments;
• related patent analysis;
• advantages and risks of development, etc.
The report is helpful for project application, drug molecule design, research progress updates, publication of research papers, patent applications, etc. If you are interested to get a full version of this report, please feel free to contact us at BD@silexon.ai
More Common Targets
TRBV18 | TRBV19 | TRBV2 | TRBV20-1 | TRBV21-1 | TRBV21OR9-2 | TRBV22-1 | TRBV23-1 | TRBV24-1 | TRBV25-1 | TRBV27 | TRBV28 | TRBV29-1 | TRBV3-1 | TRBV30 | TRBV4-1 | TRBV4-2 | TRBV4-3 | TRBV5-1 | TRBV5-2 | TRBV5-3 | TRBV5-4 | TRBV5-5 | TRBV5-6 | TRBV5-7 | TRBV5-8 | TRBV6-1 | TRBV6-2 | TRBV6-3 | TRBV6-4 | TRBV6-5 | TRBV6-6 | TRBV6-7 | TRBV6-8 | TRBV6-9 | TRBV7-2 | TRBV7-3 | TRBV7-4 | TRBV7-6 | TRBV7-7 | TRBV7-8 | TRBV7-9 | TRBV9 | TRD-AS1 | TRDC | TRDD2 | TRDD3 | TRDMT1 | TRDN | TRDV1 | TRDV2 | TRDV3 | TRE-TTC10-1 | TRE-TTC3-1 | TRE-TTC9-1 | TREH | TREM1 | TREM2 | TREML1 | TREML2 | TREML3P | TREML4 | TREML5P | TRERF1 | TRERNA1 | TREX1 | TREX2 | TRF-GAA8-1 | TRG | TRG-AS1 | TRGC1 | TRGC2 | TRGJP1 | TRGV1 | TRGV10 | TRGV2 | TRGV3 | TRGV4 | TRGV5 | TRGV5P | TRGV7 | TRGV9 | TRH | TRHDE | TRHDE-AS1 | TRHR | Triacylglycerol Lipase (TG Lipase) | TRIAP1 | TRIB1 | TRIB2 | TRIB3 | Tribbles homolog | Triggering receptor expressed on myeloid cells | TRIL | TRIM10 | TRIM11 | TRIM13 | TRIM14 | TRIM15 | TRIM16