KCNQ1: A Potent Drug Target and Potential Biomarker for Cardiovascular Disease
KCNQ1: A Potent Drug Target and Potential Biomarker for Cardiovascular Disease
Introduction
KCNQ1, a voltage-gated potassium channel subunit, is a protein that plays a crucial role in the function of excitable membranes in various organisms, including humans. This ion channel is involved in several physiological processes, including muscle contractions, nerve impulse transmission, and heart rate regulation. It is also a well-established risk factor for cardiovascular disease, which is a leading cause of morbidity and mortality worldwide.
The discovery of KCNQ1 as a potential drug target and biomarker for cardiovascular disease has significant implications for the development of new therapeutic approaches. In this article, we will provide an overview of the current research on KCNQ1, its functions, and its potential as a drug target and biomarker.
Current Research on KCNQ1
KCNQ1 is a member of the voltage-gated potassium channel subfamily, which includes several related proteins that play a crucial role in the regulation of ion traffic in excitable membranes. These channels are involved in a wide range of physiological processes, including muscle and nerve function , as well as heart rate and rhythm regulation.
Recent studies have identified several potential drug targets based on KCNQ1. These include modulating the activity of KCNQ1 to improve neuronal excitability, reducing the risk of arrhythmias, and decreasing the myocardial infarction risk.
Additionally, several research groups have used genetic modifying techniques to alter the expression of KCNQ1 and to study its role in various diseases, including heart failure, hypertension, and epilepsy. These studies have provided new insights into the biology of KCNQ1 and have identified potential drug targets.
Potential as a Biomarker
The potential use of KCNQ1 as a biomarker for cardiovascular disease has significant implications for the development of new diagnostic tests and therapies. Given its involvement in multiple physiological processes, including cardiovascular function, it is a promising marker for assessing the risk of cardiovascular disease.
Recent studies have shown that changes in the expression of KCNQ1 are associated with various cardiovascular risk factors, including age, sex, and family history. For example, studies have shown that individuals with certain genetic variations in the KCNQ1 gene are at increased risk for cardiovascular disease.
In addition, some studies have shown that modulating the activity of KCNQ1 can be an effective method for reducing the risk of cardiovascular disease. For example, one study found that inhibiting the activity of KCNQ1 using a small molecule inhibitor reduced the risk of myocardial infarction in diabetic rats.
Despite these promising findings, more research is needed to fully understand the role of KCNQ1 as a biomarker for cardiovascular disease. Further studies are needed to determine the accuracy and reliability of using KCNQ1 as a biomarker for cardiovascular disease and to develop new diagnostic tests based on this marker.
The potential for new drug research and development
The identification of a potential drug target and biomarker for cardiovascular disease has significant implications for the development of new therapeutic approaches. Given its involvement in multiple physiological processes and its association with various cardiovascular risk factors, KCNQ1 is a promising target for drug development.
Research has identified several potential drugs that can modulate the activity of KCNQ1, including inhibitors of ion channels, modulators of gene expression, and antagonists of neurotransmitters. These drugs have the potential to improve neuronal excitability, reduce the risk of arrhythmias, and decrease the risk of myocardial infarction.
In addition, some researchers have used genetic modifying techniques to alter the expression of KCNQ1 and to study its role in various diseases, including heart failure, hypertension, and epilepsy. These studies have provided new insights into the biology of KCNQ1 and have identified potential drug targets.
Conclusion
In conclusion, KCNQ1 is a voltage-gated potassium channel subunit that plays a crucial role in the regulation of ion traffic in excitable membranes. Its involvement in multiple physiological processes makes it an attractive target for drug development. Several potential drugs have been identified that can modulate the activity of KCNQ1, including inhibitors of ion channels, modulators of gene expression, and antagonists of neurotransmitters. Further research is needed to fully understand the role of KCNQ1 as a drug target and biomarker for cardiovascular disease.
Protein Name: Potassium Voltage-gated Channel Subfamily Q Member 1
Functions: Potassium channel that plays an important role in a number of tissues, including heart, inner ear, stomach and colon (PubMed:10646604, PubMed:25441029). Associates with KCNE beta subunits that modulates current kinetics (PubMed:9312006, PubMed:9108097, PubMed:8900283, PubMed:10646604, PubMed:11101505, PubMed:19687231). Induces a voltage-dependent current by rapidly activating and slowly deactivating potassium-selective outward current (PubMed:9312006, PubMed:9108097, PubMed:8900283, PubMed:10646604, PubMed:11101505, PubMed:25441029). Promotes also a delayed voltage activated potassium current showing outward rectification characteristic (By similarity). During beta-adrenergic receptor stimulation participates in cardiac repolarization by associating with KCNE1 to form the I(Ks) cardiac potassium current that increases the amplitude and slows down the activation kinetics of outward potassium current I(Ks) (By similarity) (PubMed:9312006, PubMed:9108097, PubMed:8900283, PubMed:10646604, PubMed:11101505). Muscarinic agonist oxotremorine-M strongly suppresses KCNQ1/KCNE1 current (PubMed:10713961). When associated with KCNE3, forms the potassium channel that is important for cyclic AMP-stimulated intestinal secretion of chloride ions (PubMed:10646604). This interaction with KCNE3 is reduced by 17beta-estradiol, resulting in the reduction of currents (By similarity). During conditions of increased substrate load, maintains the driving force for proximal tubular and intestinal sodium ions absorption, gastric acid secretion, and cAMP-induced jejunal chloride ions secretion (By similarity). Allows the provision of potassium ions to the luminal membrane of the secretory canaliculus in the resting state as well as during stimulated acid secretion (By similarity). When associated with KCNE2, forms a heterooligomer complex leading to currents with an apparently instantaneous activation, a rapid deactivation process and a linear current-voltage relationship and decreases the amplitude of the outward current (PubMed:11101505). When associated with KCNE4, inhibits voltage-gated potassium channel activity (PubMed:19687231). When associated with KCNE5, this complex only conducts current upon strong and continued depolarization (PubMed:12324418). Also forms a heterotetramer with KCNQ5; has a voltage-gated potassium channel activity (PubMed:24855057). Binds with phosphatidylinositol 4,5-bisphosphate (PubMed:25037568). KCNQ1-KCNE2 channel associates with Na(+)-coupled myo-inositol symporter in the apical membrane of choroid plexus epithelium and regulates the myo-inositol gradient between blood and cerebrospinal fluid with an impact on neuron excitability
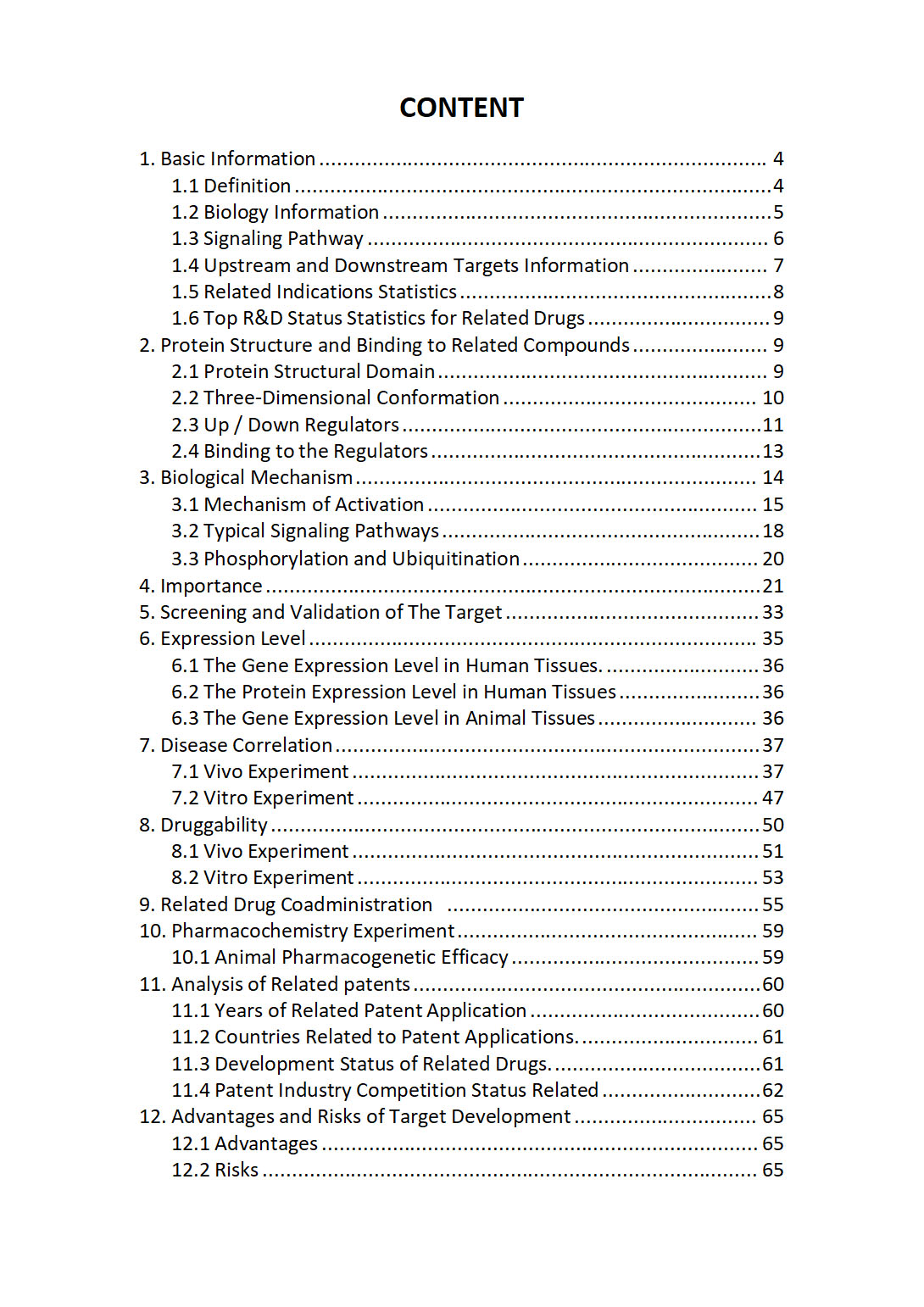
The "KCNQ1 Target / Biomarker Review Report" is a customizable review of hundreds up to thousends of related scientific research literature by AI technology, covering specific information about KCNQ1 comprehensively, including but not limited to:
• general information;
• protein structure and compound binding;
• protein biological mechanisms;
• its importance;
• the target screening and validation;
• expression level;
• disease relevance;
• drug resistance;
• related combination drugs;
• pharmacochemistry experiments;
• related patent analysis;
• advantages and risks of development, etc.
The report is helpful for project application, drug molecule design, research progress updates, publication of research papers, patent applications, etc. If you are interested to get a full version of this report, please feel free to contact us at BD@silexon.ai
More Common Targets
KCNQ1DN | KCNQ1OT1 | KCNQ2 | KCNQ3 | KCNQ4 | KCNQ5 | KCNQ5-AS1 | KCNQ5-IT1 | KCNRG | KCNS1 | KCNS2 | KCNS3 | KCNT1 | KCNT2 | KCNU1 | KCNV1 | KCNV2 | KCP | KCTD1 | KCTD10 | KCTD11 | KCTD12 | KCTD13 | KCTD13-DT | KCTD14 | KCTD15 | KCTD16 | KCTD17 | KCTD18 | KCTD19 | KCTD2 | KCTD20 | KCTD21 | KCTD21-AS1 | KCTD3 | KCTD4 | KCTD5 | KCTD5P1 | KCTD6 | KCTD7 | KCTD8 | KCTD9 | KDELR1 | KDELR2 | KDELR3 | KDF1 | KDM1A | KDM1B | KDM2A | KDM2B | KDM3A | KDM3B | KDM4A | KDM4B | KDM4C | KDM4D | KDM4E | KDM5A | KDM5A-GATAD1-EMSY chromatin complex | KDM5B | KDM5C | KDM5D | KDM6A | KDM6B | KDM7A | KDM7A-DT | KDM8 | KDR | KDSR | KEAP1 | Kelch-like protein | KERA | Keratin | KHDC1 | KHDC1L | KHDC1P1 | KHDC3L | KHDC4 | KHDRBS1 | KHDRBS2 | KHDRBS3 | KHK | KHNYN | KHSRP | KHSRPP1 | KIAA0040 | KIAA0087 | KIAA0232 | KIAA0319 | KIAA0319L | KIAA0408 | KIAA0513 | KIAA0586 | KIAA0753 | KIAA0754 | KIAA0825 | KIAA0930 | KIAA1107 | KIAA1143 | KIAA1191